The price of life is eternal vigilance. If you have severe food allergies, that is your reality. Every day, every meal, every bite. Eating is an intrinsic and essential part of what we do and who we are, so the idea that our bodies can rebel violently to everyday foods can be difficult to believe. But it’s real, and the numbers of the severely food allergic are growing. Frustratingly, we don’t know why. While recognized over 100 years ago, the social acknowledgment had lagged. That’s improved in the past decade. Food allergy prevention approaches are now a routine part of travel, school, sports, and the workplace. Peanuts on planes seem to have completely disappeared. The days of lunchbox peanut butter sandwiches are over, with many schools completely banning all peanut-containing products. It is the education system that seems to have become a ground zero for allergy programs and policies, where educators are challenged to ensure that schools are safe environments for all children, some of whom have long lists of food allergies. Continue reading
hemocode
A right way, and a wrong way, to promote the role of the pharmacist
Weekend Reading
It’s the peak of summer and much of the Eastern seaboard has been melting under record heat. Here’s some links of interest:
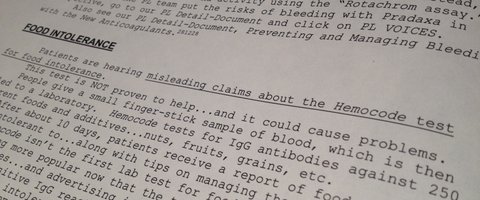
Pharmacist’s Letter issues warning about Hemocode food intolerance testing
From the December, 2012 Canadian Pharmacist’s Letter (paywalled, sorry), a subscription-funded, completely independent resource for pharmacists, comes a warning about the Hemocode food intolerance test: Continue reading
A Strong Message to Pharmacists about IgG Food Sensitivity Testing
From the Canadian Society of Allergy and Clinical Immunology:
The Canadian Society of Allergy and Clinical Immunology (CSACI) is very concerned about the increased marketing of food-specific immunoglobulin G (IgG) testing towards the general public over the past few years, supposedly as a simple means by which to identify “food sensitivity”, food intolerance or food allergies. In the past, this unvalidated form of testing was usually offered by alternative or complementary health providers, but has now become more widely available with direct-to-consumer marketing through a nationwide chain of pharmacies. Continue reading
Choosing Wisely: Five things Pharmacists and Patients Should Question

Is the health care spending tide turning? Unnecessary medical investigations and overtreatment seems to have entered the public consciousness to an extent I can’t recall in the past. More and more, the merits of medical investigations such as mammograms and just this week, PSA tests are being being widely questioned. It’s about time. Previous attempts to critically appraise overall benefits and consequences of of medical technologies seem to have died out amidst cries of “rationing!”, particularly in the United States. But all health systems are struggling to manage unsustainable cost increases. But this time, the focus has changed – this isn’t strictly a cost issue, but a quality of care issue. It’s being championed by the American Board of Internal Medicine Foundation (ABIM) under the banner Choosing Wisely with the support of several medical organizations. The initiative is designed to promote a candid discussion between patient and physician: “Is this test or procedure necessary?”. Nine organizations are already participating, represent nearly 375,000 physicians. Each group developed its own list based on the following topic: Five Things Physicians and Patients Should Question. Here are the lists published to date:
- American Academy of Allergy, Asthma & Immunology
- American Academy of Family Physicians
- American College of Cardiology
- American College of Physicians
- American College of Radiology
- American Gastroenterological Association
- American Society of Clinical Oncology
- American Society of Nephrology
- American Society of Nuclear Cardiology
ABIM has partnered with Consumer Reports to prepare consumer-focused material as well, so patients can initiate these discussions with their physicians. How did this all come to be? A candid editorial from Howard Brody in the New England Journal of Medicine in 2010:
In my view, organized medicine must reverse its current approach to the political negotiations over health care reform. I would propose that each specialty society commit itself immediately to appointing a blue-ribbon study panel to report, as soon as possible, that specialty’s “Top Five” list. The panels should include members with special expertise in clinical epidemiology, biostatistics, health policy, and evidence-based appraisal. The Top Five list would consist of five diagnostic tests or treatments that are very commonly ordered by members of that specialty, that are among the most expensive services provided, and that have been shown by the currently available evidence not to provide any meaningful benefit to at least some major categories of patients for whom they are commonly ordered. In short, the Top Five list would be a prescription for how, within that specialty, the most money could be saved most quickly without depriving any patient of meaningful medical benefit.
Health care professionals are, in general, self-regulating professions. That is, governments entrust them to set the standards for their profession and regulate members, in the public interest. Consequently, attempts by payors of services (i.e., government and insurers) to guide medical practice are usually met with substantial resistance. No-one wants insurers interfering in the patient-physician relationship. That’s why it’s exciting to see this initiative in place: It’s being driven by the medical profession itself.
As a pharmacist I’m also a member of a self-regulating profession, one in which the public places a considerable degree of trust in. In order to maintain the public’s confidence, it is essential that the pharmacy profession maintain the highest professional and ethical standards, and do its part to reduce unnecessary testing and investigations. With this in mind, I’ve taken up Brody’s challenge and developed my own list of Five things Pharmacists and Patients Should Question. While eliminating them may not provide the most savings to patients, they are pharmacy-based, widely offered, and offer little to no benefit to consumers. Here are my top five candidates: Continue reading
Food intolerance blood tests have no place in the pharmacy
Imagine your pharmacy features a blood pressure measurement device. It has never worked correctly. Sometimes it give incorrect high results, suggesting hypertension. In other patients it misses hypertension completely. You’ve been advised by hypertension experts that this particular model isn’t accurate and shouldn’t be offered to consumers. Despite this, you continue to promote it to your patients, and you use the test results to recommend supplements to treat conditions that may or may not not exist.
Does this meet the professional standards expected for pharmacists? From an ethical perspective, does it respect patient autonomy? My sense is that consumers, ethicists, regulators, and other health professionals would say “no”. Pharmacists have an ethical and professional responsibility to base advice on the best scientific evidence – in this case, to ensure that a service being offered is reliable, accurate, and relevant for making health decisions.
That’s why I’m surprised to see Canadian and American pharmacies are now selling IgG food intolerance tests. Because if you agree that knowingly offering faulty blood pressure measurement tests is unacceptable, you should have just as much concern about food intolerance blood tests. These tests have been available for some time in the United Kingdom. Now they’re in North America. Rexall, the Canadian pharmacy chain, recently started selling the “Hemocode” test which is purported to test for 250 food intolerances: Continue reading





You must be logged in to post a comment.